Exploring the Overlap Between Migraine Cervicogenic and Tension-Type Headaches
- Jason Scoppa
- 1 day ago
- 3 min read
Headaches affect millions worldwide, yet their causes and classifications often blur. Migraine, cervicogenic, and tension-type headaches are commonly treated as separate conditions. But what if they exist along a spectrum, sharing symptoms and underlying mechanisms? This idea, explored in Liblanc’s 1999 study, challenges traditional views and opens new paths for diagnosis and treatment.
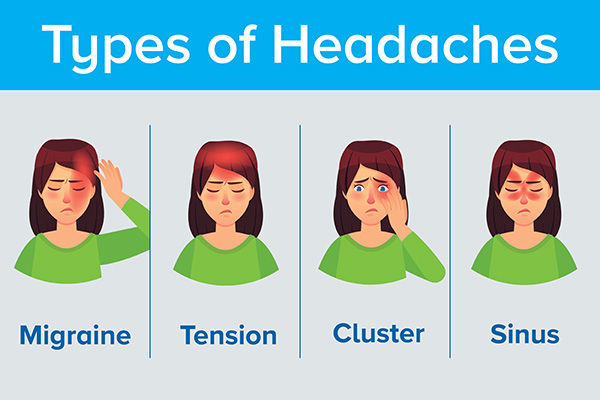
Understanding the Three Headache Types
To appreciate the possibility of a continuum, it helps to understand each headache type individually.
Migraine
Migraines are intense, often throbbing headaches, usually on one side of the head. They come with symptoms like nausea, light sensitivity, and sometimes visual disturbances called auras. Migraines can last hours to days and significantly impact daily life.
Cervicogenic Headache
These headaches originate from problems in the neck, such as joint dysfunction or muscle tightness. Pain often starts in the neck or base of the skull and radiates to the front or sides of the head. Movement or pressure on the neck can worsen symptoms.
Tension-Type Headache
The most common headache, tension-type headaches feel like a tight band around the head. They are usually mild to moderate in intensity and can last from 30 minutes to several days. Stress, poor posture, and muscle strain often trigger them.
Overlapping Symptoms and Mechanisms
Liblanc’s study highlights how these headaches share several features, suggesting they might not be entirely separate conditions.
Pain Location and Quality
While migraines often affect one side, tension-type and cervicogenic headaches can also cause unilateral pain. The quality of pain can overlap, with throbbing or pressing sensations appearing in all three types.
Neck Involvement
Neck pain is common in cervicogenic headaches but also appears in migraines and tension-type headaches. Muscle tenderness and restricted neck movement are shared symptoms.
Triggers and Aggravating Factors
Stress, poor posture, and physical strain can trigger or worsen all three headache types. This overlap points to shared pathways in how the brain and nervous system process pain.
Neurophysiological Links
Research shows that the trigeminocervical complex, a region where nerves from the neck and head converge, plays a role in all three headaches. This convergence may explain why symptoms and pain patterns overlap.
Implications for Diagnosis
Recognizing a continuum challenges the strict diagnostic categories used in clinical practice. Patients often present with mixed symptoms that don’t fit neatly into one type.
Comprehensive Assessment
Clinicians should evaluate headache history, pain characteristics, neck function, and triggers together rather than relying on rigid criteria.
Avoiding Misdiagnosis
Treating a cervicogenic headache as a migraine or vice versa can lead to ineffective management. Understanding the overlap helps tailor treatment to the individual’s specific symptom mix.
Integrated Treatment Approaches
If these headaches exist on a spectrum, treatment should address the shared mechanisms and individual differences.
Physical Therapy and Neck Care
Since neck dysfunction contributes to all three headaches, physical therapy focusing on posture, muscle strength, and joint mobility can relieve symptoms.
Medication and Lifestyle Changes
Migraine-specific medications may help some patients, while others benefit from stress management, regular sleep, and hydration.
Multimodal Strategies
Combining medication, physical therapy, and behavioral interventions often yields the best results. This approach respects the complex nature of headaches and their overlapping causes.

Real-World Example
Consider a patient who experiences frequent headaches with throbbing pain on one side, neck stiffness, and sensitivity to light. Traditional diagnosis might label this as migraine or cervicogenic headache. However, treating only one aspect may leave symptoms unresolved. A combined approach addressing neck mobility, migraine triggers, and stress management can improve outcomes.
Moving Forward in Headache Care
Liblanc’s continuum theory encourages healthcare providers to look beyond labels and focus on the full clinical picture. This perspective supports personalized care and may reduce the trial-and-error often involved in headache treatment.
Patients should feel empowered to discuss all their symptoms openly and seek care that addresses both head and neck factors. Ongoing research will continue to clarify how these headache types relate and how best to manage them.
Understanding the overlap between migraine, cervicogenic, and tension-type headaches offers a clearer path to relief. By recognizing shared symptoms and mechanisms, both patients and clinicians can work together toward more effective, integrated care. If you or someone you know struggles with frequent headaches, consider discussing this continuum approach with a healthcare professional to explore a treatment plan tailored to your unique needs.
Liblanc, "Migraine, cervicogenic and tension-type headaches - A continuum theory: Fact or fiction?", AECC Project List 1999




Comments